Lymphedema Therapy
Treatment for Lymphedema
Lymphedema is not curable, but is controllable. The aim of treatment is to improve appearance, increase function, decrease the amount of fluid in an area, decrease heaviness/achiness, and prevent further progression of the swelling. Treatment can be very effective and can greatly improve quality of life. The best and most effective treatment for Lymphedema is Complete Decongestive Therapy (CDT), which has 5 major components:
- Manual Lymphatic Drainage (MLD) is a gentle massage technique to open the collateral lymphatic pathways to assist in moving the access fluid to areas where the lymph system is functioning
- Compression Therapy/Bandaging and Garments are an essential component of Lymphedema management. Keeping the limb wrapped in a multi-layer low-stretch bandage during treatment can decrease the excess fluid, and help to soften the tissues. After treatment, a strong gradient compression stocking or sleeve can help in maintaining results.
- Exercising according to recommended CDT protocols can help stimulate the lymphatic system to get fluid moving
- Skin & Nail Care is crucial on the affected limb to prevent skin cracking. Using low pH soaps and lotions can help protect against bacterial infections (which can lead to cellulitis)
- Comprehensive Health Management and excellent nutrition is also important. Controlling weight is necessary as studies have found that obesity aggravates Lymphedema.
If you would like to learn more about Lymphedema or Lymphedema Compression Garments, please use the buttons below:
Niagara Lymphedema Therapy / Complete Decongestive Therapy Rates
1½ Hour Initial Assessment: $175
1 Hour Follow Up Appointment: $105
45 Minute Follow Up Appointment: $90
1 Hour Post-Surgery/Plastic Surgery Appointment: $125
ADP Assessment 30 min: $75
Cancellation Policy:
There will be a 50% cancellation fee applied to any missed appointments or appointments cancelled with less than 24 hours’ notice. Our late cancellation fee will be waived if you cancel due to illness or suspected illness. We would prefer to reschedule your appointment if you are ill. Please try to give our office appropriate notice.
Additional Lymphedema Information
Contents
What is Lymphedema?
Symptoms of Lymphedema
Are you at Risk?
Breast Cancer Related Lymphedema
Lower Extremity Lymphedema
Treatment for Lymphedema
Upper Extremity Lymphedema Therapist: Beth Elliott, R.M.T., CLT-LANA
Rates for Niagara Lymphedema Therapy / Complete Decongestive Therapy
What is Lymphedema?
Lymphedema is a swelling of a body part (arm, leg, breast/trunk, head, face & neck or genitals) It is caused by an abnormal accumulation of fluid, proteins and cellular waste in the tissues under the skin. Lymphedema is caused by an imbalance between the normal amount of lymph fluid and reduced capacity that the vessels are about to transport. This results in accumulation of protein-rich fluid.
It occurs when there is a disruption in the lymphatic system such as:
- failure of the lymph vessels to develop properly and you are born with abnormalities in the lymphatic system – known as Primary Lymphedema.
- damage to lymph vessels by trauma, surgery, radiation or infection- known as Secondary Lymphedema.
- Removal or destruction of lymph nodes, usually as a result of cancer treatment (surgery and/or radiation).
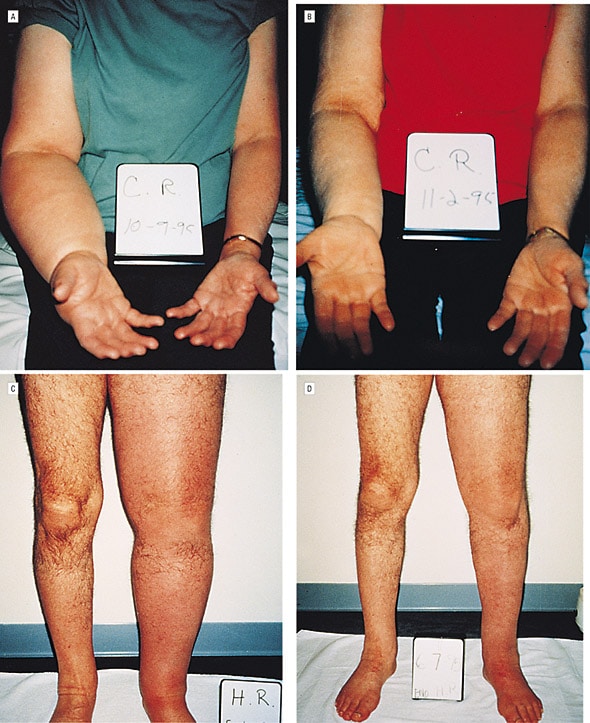
before and after Complete Decongestive Therapy (CDT)
Symptoms of Lymphedema:
- fullness, heaviness and achiness sensation in the limb
- skin feeling tight
- decreased flexibility
- swelling in a specific area
- redness- the appearance of redness, rashes or heat in the at-risk
- limb thickening of the skin
- hardening of the limb
- leakage of lymph through the skin
- excessive swelling
Are you at Risk?
Lymphedema most commonly follows a surgical procedure in which there has been a removal or disruption of the lymph nodes or vessels.
If you have been exposed to any of the following procedures or situations, you may be at risk for developing Lymphedema.
- biopsy of Inguinal (groin) or Axillary (armpit) Lymph Nodes
- breast surgery or Prostate surgery
- radiation or Chemotherapy treatment
- other surgery involving lymph nodes
- broken limbs from trauma
- hernia repair
- venous Insufficiency
- severe infections
- other medical procedure involving the lymphatic system.
Lower Extremity Lymphedema
Lymphedema is a disease, not a symptom, of an underlying malresponsive lymphatic system that is unable to clear protein fluids from the space that suspends all the cells. There are numerous causes of lower extremity lymphedema.
- Primary Lymphedema: These are individuals who are born with the disease of lymphedema. Often people with hereditary conditions are born with impaired lymphatic systems and thus born with lymphedema, such as: Millroy’s disease, Meige’s disease, Turner’s syndrome and Noonan’s syndrome. They often exhibit lower limb bilateral swelling.
- Secondary Lymphedema: This is when a symptom of edema causes the disease of lymphedema and/or is manufactured due to poor health conditions or through treatment of cancer. This over time with no intervention can become an irreversible failure of the lymphatic system. Below, in order, are the leading causes of lymphedema.
- Obesity: Due to fatty-tissue proliferation with increased inflammation triggers a cascading effect of lymphatic uptake failure and increasing hardening of soft tissues and skin that immobilizes the lymph fluid.
- Chronic Venous Insufficiency: Due to the vein’s valves inability to contain fluid a pooling of blood occurs and creates a retrograde flow (fluid back-up) in the surrounding tissues; thus, creating swelling.
- Congestive Heart Failure: Due to the heart’s inability to effectively pump or fill the chambers a pooling of fluid begins to occur. Often this can be seen in the feet and ankles first. These patients might also experience orthopnea, hard time breathing laying down, due to the pooling of fluid in the lungs. These patients often like to sleep on recliners.
- Treatment of Cancer/Iatrogenic (dissection/node removal, radiation): Surgical intervention of cancer can sometimes mean lymph nodes are to be removed as the cancer spreads. This mechanically dampens the lymphatic systems ability to drain protein fluids, thus creating lymphedema. Radiation treatment to cancer can also have lymphatic impairment causing blockage and thus inhibiting regular drainage of the lymph.
- Lipedema: Is a disorder of fatty metabolism that almost exclusively occurs in women. This is not lymphedema but lipedema and lymphedema are often found to co-exist in a patient. These patients do not exhibit swelling of the legs, unless they have lymphedema, but show disproportionate fatty deposition at the hips, thighs and legs while the feet remain unaffected.
The treatment protocol for lower extremity lymphedema is to provide Complete Decongestive Therapy (CDT) involving a phase of decongestion and a phase of maintenance. This includes Manual Lymphatic Drainage (MLD) of affected regions, thereby manually moving the fluid back into circulation and decreasing volume of the affected regions. Once manually drained, compression bandaging/therapy is applied to maintain the reduced size in order to continue the decongestive work.
Upper Extremity Lymphedema Therapist: Beth Elliott, R.M.T, CLT-LANA
Qualifications:
- Registered Massage Therapist since 1996
- Specializing in Breast Cancer-related Lymphedema
- Certified Lymphedema Therapist- CLT- 135 hour extensive training in Complete Decongestive Therapy (CDT) with Klose Training-Corning NY
- Breast Cancer Rehabilitation Course-Klose Training
-
- This course provides essential knowledge of outpatient therapeutic approaches in breast cancer care. A comprehensive review of current diagnostic, surgical, radiation, reconstructive and medical oncologic management for breast cancer is included. Special attention is given to the evaluation, differential diagnosis, and treatment of axillary web syndrome (cording) and postural and scapular dysfunction as well as upper-quadrant soft-tissue changes following breast cancer surgery and radiation therapy. An up-to-date review of recent research findings regarding breast cancer-related lymphedema is presented.
- LANA (Lymphology Association of North America) Certified in Lymphedema
- Assistive Device Program (ADP) Authorizer Status for Lymphedema Compression Garments
Who are Certified Lymphedema Therapists-LANA?
CLT-LANA therapists are healthcare professionals who have successfully passed a comprehensive examination by demonstrating knowledge about the lymphatic system and Lymphedema management. CLT-LANA credentials confirm for patients and referring medical providers that the therapist has the highest level of competency in the profession and has remained current with advancements in the field.
Lymphedema Compression Garments for the Management of Lymphedema
Beth Elliott RMT-CLT-LANA is a Registered Authorizer for Assistive Device Program (ADP)
Assistive Devices Program (ADP)
The Assistive Devices Program (ADP) of the Ministry of Health and Long-Term Care provides funding assistance for Pressure Modification Devices (PMD)—compression garments and sleeves—for chronic lymphedema management as well as sequential extremity pumps for primary lymphedema management. Any resident of Ontario with a valid Ontario health card is eligible to apply. The ADP pays 75% of the approved cost. Those receiving benefits from certain social assistance programs may be eligible for 100% funding of the approved cost. An Application for Funding Pressure Modification Devices form can be obtained from an ADP registered authorizer or vendor or downloaded and printed from the ADP website.
Funding for Pressure Modification Devices – Information Sheet (PDF)
Summary of Application Process
- Book an ADP Assessment with Beth Elliott RMT, CLT-LANA, Registered Authorizer ADP to assess and discuss the garment required for the management of your Lymphedema. The Authorizer will answer any questions and fill out the application to authorize and direct you to a Registered Fitter and Specialist to assist with the application process.
- Have an ADP Approved Specialist sign and date the application to confirm a diagnosis of Lymphedema. The list of approved specialists: Doctors or specialists that can examine you, diagnose you and sign your application form must practice in one of the following areas:
- cardiovascular surgery
- vascular surgery
- orthopedic surgery
- radiation oncologymedical oncology
- internal medicine
- pediatrics
- physiatry
- plastic surgery
- general surgery
- Have an ADP Registered Fitter measure and provide garments appropriate for the client. Have the registered vendor invoice ADP for 75% and invoice the client for the remaining 25%
ADP Information
For more information on the ADP, you can visit the following page at: www.ontario.ca/page/assistive-devices-program
You can email ADP directly at adp@ontario.ca
Alternately, you may call the ADP at 416-327-8804, toll free at 1-800-268-6021 or TTY at 1-800-387-5559.
The ADP Authorization assessment is 30 minute appointment at a cost of $75.00